Posterior Cervical Fusion
As we age, degenerative changes in the discs, bones, and ligaments of our spine can cause a narrowing of the canal that the spinal cord runs through. Sometimes, this narrowing of the spinal canal, also called spinal stenosis, is present from birth (congenital). Spinal stenosis can lead to compression of the spinal cord that can cause a varying degree of symptoms. Symptoms caused by pressure on the cervical spinal cord include difficulty with balance and walking, decreased fine motor function of the hands, numbness or weakness of the hands or arms, and neck pain. Spinal stenosis is a progressive disease that can continue to worsen with time.
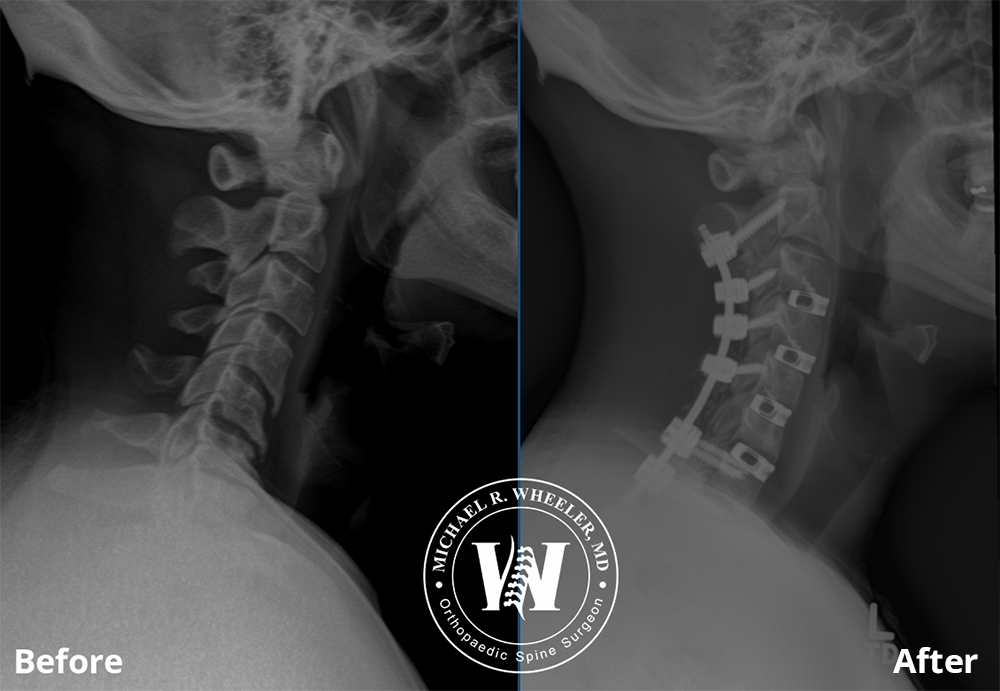
One surgery used to treat cervical stenosis is a posterior cervical decompression and fusion. Decompression in this setting means relieving the pressure off the effected spinal cord or nerves. Posterior cervical fusion is a way to provide multiple-level stabilization of the bones of the spine from the back of the neck.
Benefits of posterior cervical decompression and fusion
- Relief of symptoms caused by cervical spinal stenosis
Posterior cervical decompression and fusion allows for direct decompression of the spinal cord and nerves that are being compressed by diseased disc, bone, or ligament. By removing the pressure off the cord and/or nerves, the symptoms the patient is experiencing should improve. - Pain relief
By relieving the pressure off the spinal cord and effected nerve roots, chronic pain caused by the stenosis should be partially or completely relieved. By relieving the pressure off the spinal cord and stabilizing the bones, quality of life can be drastically improved. - Correction of posture or poor alignment
As we age, degenerative changes of the spine can lead to abnormal curvature of the spine. This is usually seen in the form of kyphosis. Posterior cervical fusion can help realign the spine and restore cervical lordosis (the proper curvature of the cervical spine). This will improve the patient’s posture, allowing them to stand up straighter and relieve stress on the neck and shoulders.
Patients who would benefit from posterior cervical decompression and fusion
- Patients with cervical spinal stenosis (narrowing of the spinal canal in the neck that the cord runs through) with symptoms that affect daily life.
- Patients with cervical spinal stenosis that have progressive symptoms of difficulty with balance and walking, decreased fine motor function of the hands, numbness or weakness of the hands or arms, or neck pain. This is called cervical myelopathy.
- Patients who have already had cervical fusion using an anterior approach (surgery from the front of the neck) and either continue to have symptoms from spinal stenosis or have had failure of fusion of the bones.
Procedure
For posterior cervical decompression and fusion, the patient is positioned prone (or face-down) on the operating table with lots of padding to protect the face and other bony areas. Advanced monitoring of the nerves and spinal cord is used throughout the entire surgery that allows for safe monitoring of each nerve and its function. This monitoring technique is called intra-operative neuro monitoring and is used for the patient’s safety.
An incision is made on the back of the neck over the affected level(s). After the vertebrae (bones) have been exposed, screws and rods are carefully placed for stabilization. If necessary, small pieces of bone are removed to allow decompression (or relief of pressure) of the spinal cord and/or nerves.
Bone graft is then placed to help promote fusion of the bones. The bone graft is usually a combination of the patient’s own bone and bone from cadaver.
The incision is then closed using absorbable suture and a dressing is placed. Occasionally, a drain may be left in place to prevent fluid accumulation within the wound.
Postoperative recovery
The recovery time for posterior cervical fusion surgery varies widely, but it can take 3-6 months to feel fully recovered. A combination of pain medicine, rest, and physical therapy will help aid in recovery. Avoiding bedrest after surgery is important. Although there will be some limitations to activity, staying mobile is key to a healthy recovery.
Risks and possible complications
- Wound complications
As with any surgery, wound infection can occur. Keeping the incision clean and dry will help reduce risk of infection. Smoking, history of infection, obesity, poor nutrition, and other chronic health problems such as diabetes can impede wound healing and increase risk of complications.
- Nerve damage
Although rare, it is possible to sustain an injury to the spinal nerves during the surgery. Neuro monitoring is used to detect any change in function of the nerves during surgery and identify any problems before leading to nerve damage.
- Lack of improvement in symptoms
Depending on the severity and duration of spinal stenosis, the nerve damage that has developed over time may be irreversible. Despite relieving the pressure off the nerves with surgery, sometimes permanent damage has already occurred. Surgery will still benefit the patient, because it will prevent further decline in the patient’s function over time.
- C5 palsy
Rarely after cervical decompression and fusion, the patient can have a weakness or inability to use the shoulder muscles. This is called a C5 palsy. This weakness is almost always temporary. Symptoms often resolve after a few days, but sometimes can last for a couple of months.
- Vertebral artery injury
Another rare complication of posterior cervical fusion and decompression is vertebral artery injury. There is a blood vessel in the neck near the spine, called the vertebral artery, that can be damaged during the surgery. If this vessel is damaged, there is risk for stroke.
- Failure of bones to fuse
The failure of the vertebrae (bones) to fuse is called pseudoarthrosis. Smoking, history of infection, obesity, poor nutrition, osteoporosis, and other chronic health problems such as diabetes can increase the risk of pseudoarthrosis.
- Hardware failure
After surgery, it is possible the screws and rods can break, loosen, or pull out of the bone. Smoking, history of infection, obesity, poor nutrition, osteoporosis, and other chronic health problems such as diabetes can increase the risk of hardware failure.